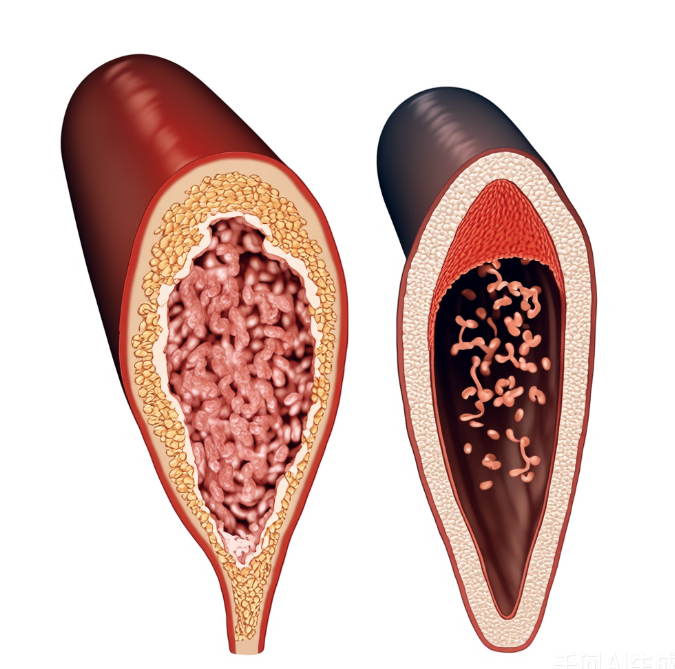
Imagine your blood vessels as a vast network of highways running through a bustling city. In youth, they’re supple and smooth—like freshly paved asphalt—allowing blood to flow freely. But over time, “road debris” such as cholesterol and triglycerides can build up, narrowing lanes or even causing traffic jams. Fortunately, your kitchen holds a natural “road maintenance crew.” Eating the right foods daily is like giving your blood vessels a spa treatment—from the inside out.
1. Fatty Fish: The “Rust Preventer” for Blood Vessels
- Eat fatty fish 2–3 times per week. Rich in omega-3 fatty acids, these healthy fats act like street sweepers, helping lower levels of “bad” LDL cholesterol in your bloodstream.
- Opt for palm-sized portions—this controls intake while minimizing exposure to heavy metals that can accumulate in larger fish.
- Steam gently to preserve nutrients; a squeeze of lemon adds freshness without overpowering the delicate flavor.
- Avoid deep-frying—high heat destroys beneficial compounds and creates substances that harm vascular health.
2. Oats: The “Robotic Vacuum” for Arteries
- A bowl of oatmeal delivers beta-glucan, a soluble fiber that forms a gel-like mesh in your gut, binding excess cholesterol like a magnet and escorting it out of your body.
- Choose steel-cut oats when possible—they take longer to cook but have a lower glycemic index. If you’re short on time, go for plain instant oats (check the label—skip added sugars!).
- Boost flavor naturally with blueberries or banana slices, but skip sugary syrups—they undo all the benefits.
3. Nuts: The “Emergency Repair Kit”
- Just a small handful (about 15g) per day provides heart-healthy unsaturated fats that keep blood flowing smoothly—like natural lubricant for your circulatory system.
- Pick raw, unsalted, in-shell nuts—the act of shelling slows you down, helping prevent overeating.
- Rotate varieties: almonds, walnuts, and Brazil nuts each offer unique nutrients, giving your vessels a well-rounded boost.
4. Green Tea: The “Pressure Release Valve”
- Packed with catechins, powerful antioxidants that protect the delicate lining of your blood vessels—think of it as applying a protective coating to your internal highways.
- Brew with water around 80°C (176°F) and steep for 3 minutes. Boiling water or over-steeping releases too much caffeine and bitterness.
- If you have a sensitive stomach, drink mild tea 30 minutes after meals to avoid interfering with iron absorption.
5. Dark Chocolate: The “Mood-Boosting Guardian”
- Choose dark chocolate with at least 70% cocoa. Its flavonoids help maintain vessel elasticity and support healthy circulation.
- Stick to about 20g per day—roughly two small squares—to satisfy cravings without excess calories.
- Let it melt slowly on your tongue rather than chewing; this enhances flavor perception and helps control portion size.
6. Garlic: The “Natural Disinfectant”
- Crush or chop garlic and let it sit for 10 minutes before cooking. This activates allicin, a potent anti-inflammatory compound that supports vascular health.
- Can’t handle raw garlic? Try garlic infused in low-heat oil—it’s gentler on the stomach yet still nutrient-rich.
- Best consumed at dinner to avoid daytime breath issues. Those with sensitive digestion should use it in moderation.
These six foods form an all-star team for vascular wellness. You don’t need fancy supplements or gourmet meals—just smart, consistent choices. Try this simple daily plan:
- Breakfast: Oats topped with berries and a few nuts
- Lunch: Grilled salmon with a side of greens + a cup of green tea
- Afternoon snack: A square or two of dark chocolate
- Dinner: Stir-fry or soup seasoned generously with fresh garlic
Stick with it for three months, and your next check-up might reveal something remarkable: your “vascular age” could be younger than your actual age.
Your heart—and your highways—will thank you.